Antimicrobial Resistance is a looming global health challenge. It takes the deadly form when microbes mutate and develop resistance to the very medicines designed to destroy them. However, hope abounds in a powerful, targeted strategy known as Antimicrobial Stewardship. AMS programs aim to ensure the optimal selection, dosing, and duration of antimicrobial treatment.
They aspire to drive change in prescribing behavior, reduce unnecessary use of antibiotics, and improve patient health outcomes. It all begins with adopting a prudent approach to antibiotic prescription and use, and here’s how:
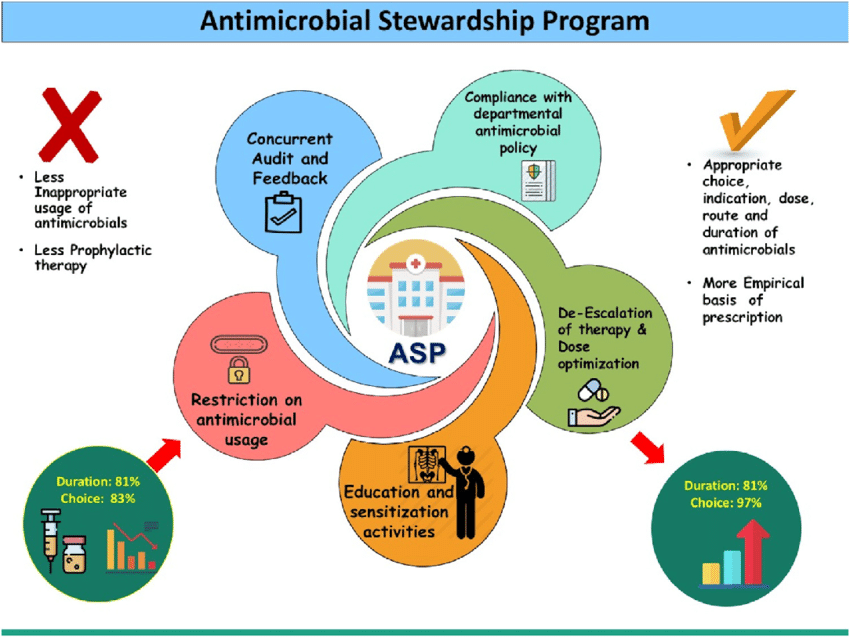
1. Optimizing Antimicrobial Prescriptions: AMS encourages healthcare providers not to rush into prescribing antibiotics, but to make careful, considerate choices regarding the right drug, optimal dosage, and suitable duration of therapy. This judicious approach not only improves patient outcomes but also minimizes the risk of developing antibiotic resistance.
2. Emphasizing Education: AMS programs play a significant role in educating both healthcare professionals and patients about the proper antibiotic use and the potential pitfalls of misuse. Understandings of when antibiotics are necessary, the significance of adhering to the prescribed dosage, and the importance of completing courses are all crucial to reducing unnecessary exposure to antibiotics, thus preventing the evolution of resistance.
3.Continuous Monitoring and Reporting: Tracking the use of antimicrobials within healthcare settings provides critical insights into prescribing habits, patterns of resistance, and overall effectiveness of the stewardship interventions. Regular feedback can encourage compliance with recommended practices and help identify areas that need improvement.
4.Enforcing Reassessment of Therapy: Ongoing reevaluation of the initial antibiotic selection is an often overlooked but critical component of AMS programs. This strategy promotes the transition from broad-spectrum antibiotics to narrower agents and encourages the de-escalation or termination of therapy when infection is ruled out. This constant revaluation helps in reducing the unnecessary antibiotic usage.
5.Supporting Non-Antibiotic Strategies: AMS advocates for the use of non-antibiotic measures such as vaccines and infection control practices. These approaches can decrease the prevalence of infections requiring antibiotic treatment, thereby reducing the overall use of antibiotics.
In summary, if intelligently implemented, AMS programs can robustly combat the growing threat of antimicrobial resistance. It takes deliberate and collective effort from all parties involved, including healthcare professionals, patients, and policy-makers. By working together, we can preserve the potency of our current antibiotics, ensuring they remain an effective tool for treating infectious diseases for generations to come. Stepping up to antimicrobial stewardship is not merely an option, but a necessity in our fight against antimicrobial resistance. Let’s commit to using antibiotics responsibly and making the world a safer place for all of us.