The emergence of antimicrobial tolerance and resistance presents a significant challenge to global public health, particularly due to the persistence of bacterial cells that can survive antibiotic treatments. This study systematically explores the interactions between various metabolic inhibitors—such as chloramphenicol (CAM), rifampicin (RIF), arsenate (ARS), and thioridazine (TDZ)—and the antibiotic ofloxacin (OFX) to understand their potential synergistic or antagonistic effects on antibiotic-tolerant persister cells. By employing multiple treatment conditions and synergy models, the research aims to elucidate the mechanisms by which these inhibitors influence bacterial survival and persistence.
Methods
This cross-sectional prospective study examined the interactions between metabolic inhibitors (chloramphenicol, rifampicin, arsenate, thioridazine) and ofloxacin in various bacterial strains under pre-, co-, and post-treatment conditions. Synergistic effects were assessed using four distinct synergy models, and multivariable linear regression analyses were conducted to evaluate correlations with cellular energy metabolism. Both conventional culture and multiplex real-time PCR were employed for bacterial identification and antimicrobial susceptibility testing.
Key Findings
- Synergy and Antagonism:
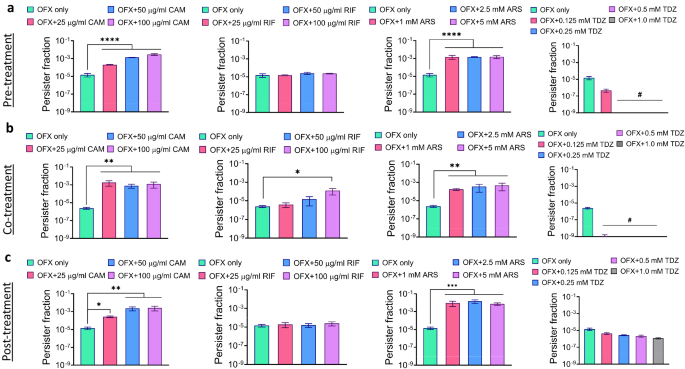
- Chloramphenicol (CAM), rifampicin (RIF), and arsenate (ARS) consistently exhibited minimal synergy scores with OFX, indicating antagonistic effects across all conditions and models.
- Thioridazine (TDZ) showed high synergy scores, particularly in pre- and co-treatment conditions, suggesting a strong synergistic effect with OFX.
- Effect on Cellular Energy Metabolism:
- Multivariable linear regression analysis revealed a correlation between TDZ’s ability to suppress cellular energy metabolism and its high synergy scores with OFX.
- ARS treatment reduced ATP levels under pre-treatment conditions but did not significantly deplete cellular energy compared to PMF inhibitors.
- Impact of Treatment Timing:
- TDZ’s synergistic effects were most pronounced during pre- and co-treatment, while its synergy decreased during post-treatment.
- The timing of metabolic inhibitor administration influenced their interactions with OFX and their effectiveness against antibiotic-tolerant cells.
- Mechanisms of Action:
- TDZ’s disruption of the proton motive force (PMF) was identified as a key factor in its ability to enhance the efficacy of OFX.
- CAM, RIF, and ARS potentially induced dormancy in bacterial cells, enhancing their survival rather than eradication.
This study highlights the complex interactions between metabolic inhibitors and antibiotics in targeting antibiotic-tolerant persister cells. These findings underscore the importance of evaluating the timing, concentration, and mechanisms of action of metabolic inhibitors to develop effective strategies against persistent bacterial infections.
Link to the study : https://tinyurl.com/68zty454