Migraine is a prevalent neurological disorder characterized by recurrent episodes of severe headache, often accompanied by nausea, vomiting, and heightened sensitivity to light and sound. Emerging evidence suggests that migraine involves complex metabolic processes and is influenced by the gut microbiome and dietary habits.
This study explores the relationship between diet, the gut microbiome, and migraine, emphasizing the interplay between these factors and their impact on migraine pathogenesis and management.
Key Findings
Dietary Factors and Migraine Triggers
Caffeine and Alcohol: These substances are identified as common dietary triggers for migraine. Excessive caffeine intake and alcohol consumption, particularly red wine, can provoke migraine episodes. Moderation and consistent consumption patterns are recommended.
Nutrients that Alleviate Migraine: Magnesium and riboflavin (vitamin B2) have been shown to help alleviate migraine symptoms. High intake of these nutrients is associated with reduced frequency and severity of migraines.
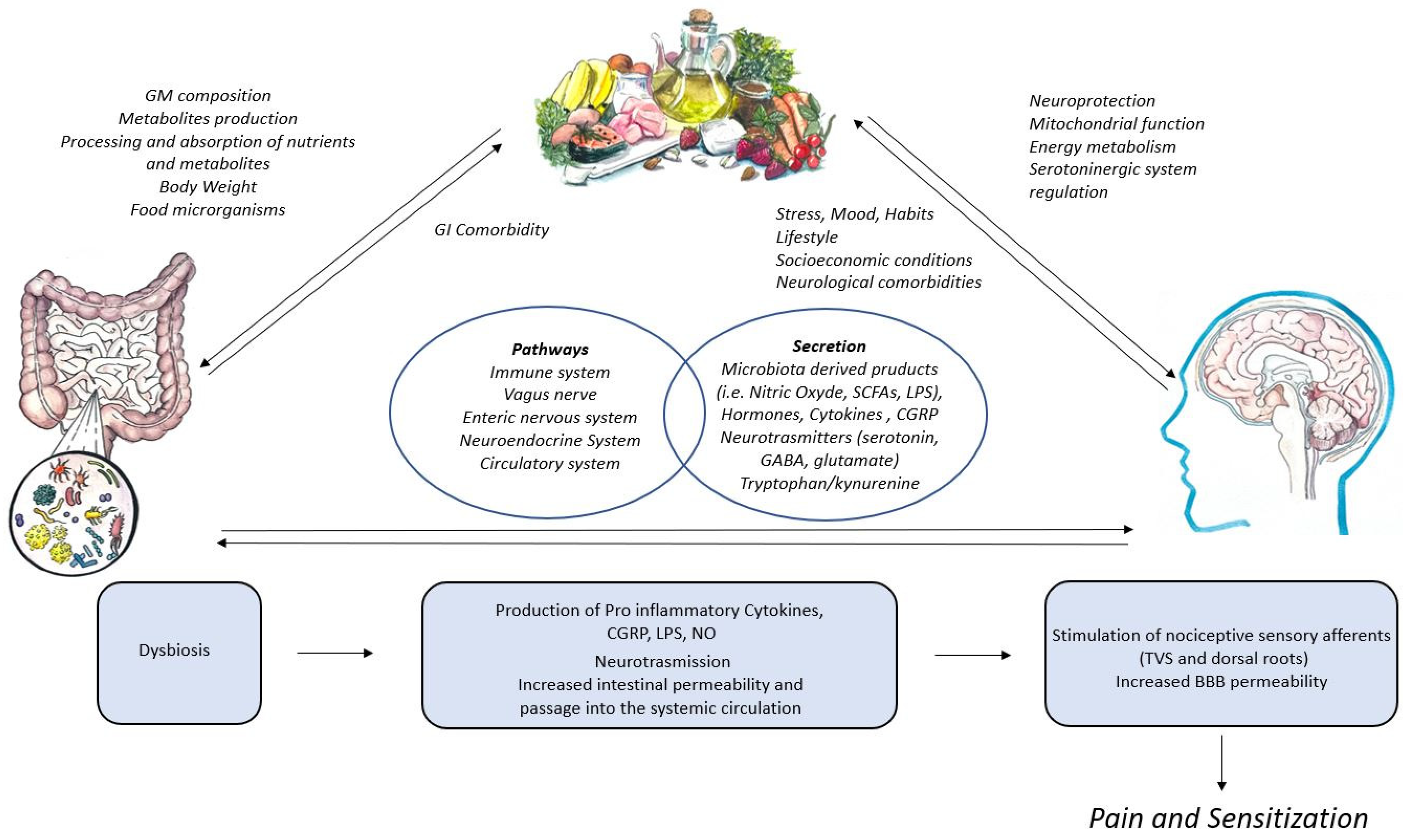
Neuroinflammation and Gut-Brain Signaling: The gut microbiome influences neuroinflammation through the vagus nerve and cytokine production. It also affects gut-brain signaling, including the production of neurotransmitters like gamma-aminobutyric acid (GABA).
Metabolic Function: Microbial metabolites such as short-chain fatty acids (SCFAs) play a crucial role in maintaining metabolic function and influencing migraine susceptibility. Dysbiosis, or microbial imbalance, is linked to increased migraine risk.
Altered Eating Patterns: Migraine can lead to poor nutritional choices and irregular eating habits due to symptoms like nausea and vomiting, which can exacerbate the condition and affect overall health.
Individual Variability: There is significant individual variability in how diet affects migraine, influenced by genetic, environmental, and lifestyle factors. Personalized dietary interventions are necessary to manage migraine effectively.
Holistic Management: Integrating dietary management, gut health optimization, and lifestyle modifications can offer a holistic approach to reducing migraine frequency and severity. This can improve patient outcomes and quality of life.
Trigeminovascular System: The activation of meningeal nociceptors within trigeminal and upper cervical nerves generates migraine pain, with the release of vasoactive mediators like CGRP, PACAP, substance P, and neurokinin-A.
CGRP and Inflammation: CGRP plays a significant role in meningeal neurogenic inflammation, which is a key factor in migraine pathogenesis. Anti-CGRP treatments have shown clinical success in reducing migraine symptoms.
Gut Microbiome and Neurological Function: The gut microbiome impacts neurological function through the production of metabolites like SCFAs, modulation of neurotransmitters, and regulation of immune responses. These factors contribute to the central and peripheral sensitization associated with migraine.
Therapeutic Interventions: Prebiotics and probiotics, lifestyle modifications (e.g., SEEDS – Sleep, Exercise, Eating, Diary, Stress reduction), and potentially fecal microbiome transplantation (FMT) are explored as therapeutic interventions for managing migraine.
By exploring these findings, this review underscores the importance of considering diet and gut health in the comprehensive management of migraine, providing insights into potential targets for intervention and lifestyle modifications to mitigate migraine symptoms.
Link to the article : https://tinyurl.com/48835xcf