Parkinson’s disease (PD) is a neurodegenerative disorder that has been increasingly linked to alterations in gut microbiota. This study aims to identify common gut microbial features in PD across different countries by meta-analyzing fecal shotgun sequencing data from Japan and five previously reported datasets from the USA, Germany, China, and Taiwan. By examining gut microbiota composition, metabolic pathways, and metabolomic profiles, the study seeks to uncover potential mechanisms by which gut dysbiosis contributes to PD pathology.
Methods
- Datasets: Fecal shotgun sequencing data from 94 PD patients and 73 controls in Japan were combined with five datasets from the USA, Germany, Shanghai, Xiangyang, and Taiwan.
- Microbial Analysis: α-Diversity and taxonomic composition were analyzed across datasets. Pathway analysis was performed to identify significantly altered metabolic pathways.
- Metabolomics: Gas chromatography-mass spectrometry (GC-MS) and liquid chromatography-tandem mass spectrometry (LC-MS/MS) assays were used to quantify fecal short-chain fatty acids (SCFAs) and polyamines.
- Correlation Analysis: Relationships between microbial gene abundances and fecal metabolite concentrations were examined.
Key Findings
Increased α-Diversity in PD: The study found a significant increase in α-diversity at the species level in PD patients across six datasets, which is unusual as most diseases tend to show decreased α-diversity.
Taxonomic Shifts: Specific microbial species showed consistent changes in abundance:
- Increased: Akkermansia muciniphila
- Decreased: Roseburia intestinalis and Faecalibacterium prausnitzii
Metabolic Pathway Changes:
- Significant decreases in genes involved in the biosynthesis of riboflavin (vitamin B2) and biotin (vitamin B7) were observed in PD.
- Five out of six categories of carbohydrate-active enzymes (CAZymes) were decreased in PD.
Decreased Metabolites:
- Fecal concentrations of SCFAs and polyamines were significantly decreased in PD patients.
Correlation with Metabolites:
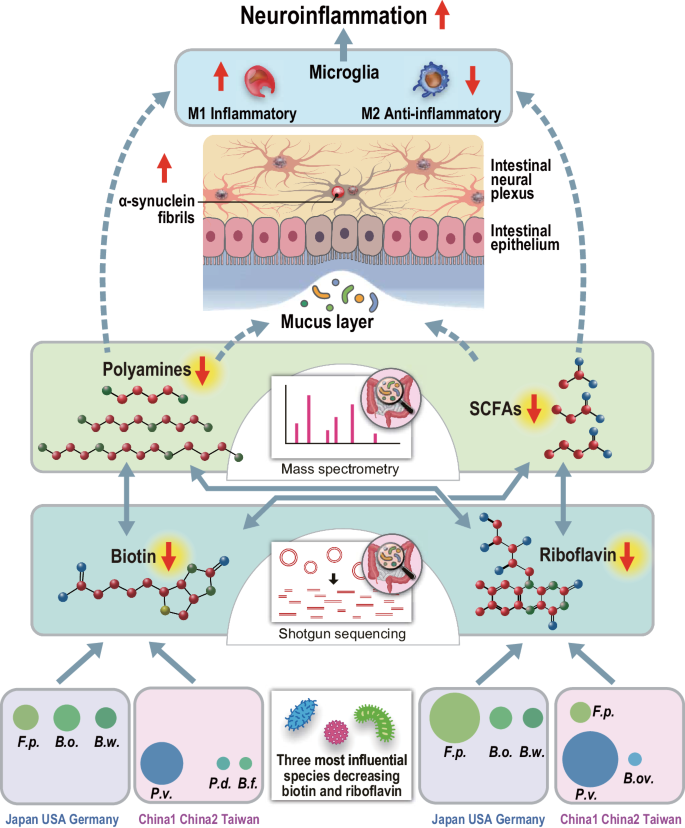
- Positive correlations were found between the genes involved in riboflavin and biotin biosynthesis and the fecal concentrations of SCFAs and polyamines.
Geographical Variations:
- The bacteria responsible for decreased riboflavin and biotin biosynthesis varied between countries, indicating geographical differences in gut microbial compositions.
Speculative Mechanisms:
- The study hypothesizes that decreased SCFAs and polyamines may lead to a thinner intestinal mucus layer, increased intestinal permeability, and subsequent neuroinflammation and α-synuclein aggregation in the intestinal neural plexus.
This comprehensive meta-analysis reveals significant alterations in gut microbiota composition and metabolic functions in PD patients. The findings suggest that decreased biosynthesis of riboflavin and biotin, along with reduced levels of SCFAs and polyamines, may play crucial roles in PD pathology by affecting gut integrity and promoting neuroinflammation. Supplementation with riboflavin and biotin could potentially benefit PD patients by mitigating these effects. Further research is needed to explore these therapeutic possibilities and understand the complex interactions between gut microbiota and PD.
Link to the study : https://tinyurl.com/ye6zt72t