Autism Spectrum Disorder (ASD) is a multifactorial neurodevelopmental disorder marked by challenges with social interaction, repetitive behaviors, and communication deficits. ASD affects approximately one out of every 100 children worldwide. Individuals with ASD often have dysregulated gut microbial balance and reduced intestinal barrier function. This study intends to investigate the mechanisms behind these interactions, with a special emphasis on the impact of probiotics, specifically Clostridium butyricum, on intestinal barrier function and behavioral outcomes in ASD mice models.
Methods – Animal Models: The study used two popular mouse models for ASD:
- BTBR T+ Itpr3tf/J (BTBR) mice: An inbred strain that exhibits behavioral impairments associated with Autism.
- Valproic Acid (VPA) mice: Developed after prenatal exposure to the antiepileptic medication valproic acid, which causes ASD-like symptoms.
- Experimental Groups: Mice were separated into two groups: control and experimental, with the latter given Clostridium butyricum therapy.
- Assessments: –
- Intestinal Barrier Function: Measures intestinal permeability and tight junction protein expression (claudin1, claudin3, and occludin).
- Inflammatory Markers: They measured IL-6, TNF-α, and IFN-γ levels.
- Microbial Analysis: The gut microbiota composition was examined to determine microbial changes.
- Behavioral Analysis: Behavioral anomalies were investigated to identify the impact of C. butyricum treatment.
Key Findings:
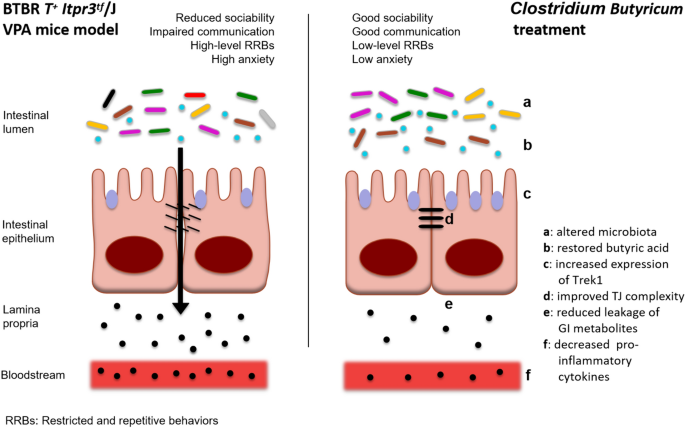
Altered Intestinal Barrier in ASD Models
- Both BTBR and VPA mice exhibited increased intestinal permeability and decreased expression of tight junction proteins (claudin1, claudin3, and occludin).
- Increased levels of pro-inflammatory cytokines (IL-6, TNF-α, and IFN-γ) indicate intestinal barrier breakdown.
Microbial Dysbiosis: Both ASD models showed significant changes in gut microbiota, such as increased Firmicutes/Bacteroidetes ratio and changes in specific bacterial taxa.
- BTBR mice showed a distinct microbial profile that had minimal diversity, while both BTBR and VPA mice displayed a higher relative abundance of Lactobacillales and decreased abundance of Erysipelotrichales and Spirochaetales.
Clostridium butyricum therapy enhances intestinal barrier function by decreasing permeability and boosting tight junction protein expression.
- The therapy also lowered the expression of histone deacetylase 1 (HDAC1) and improved intestinal barrier function via the Trek1 channel.
- Treated mice demonstrated behavioral changes, including increased exploratory behavior and decreased repetitive behavior.
Short-Chain Fatty Acids (SCFAs): ASD mice had altered SCFA profiles, including reduced levels of butyric acid.
- C. butyricum administration elevated butyric acid levels, which helped to improve gut health and behavioral outcomes.
Trek1 Channel: – ASD models showed decreased expression of the Trek1 channel, indicating a function in intestinal barrier integrity.
- C. butyricum therapy restored Trek1 expression and decreased inflammation, indicating its therapeutic potential.
This study provides substantial proof for an association of intestinal barrier dysfunction and microbial dysbiosis in ASD. The findings imply that probiotics, such as Clostridium butyricum, can enhance gut health and alleviate ASD-related behavioral issues. More research is needed to completely understand the underlying mechanisms and investigate the findings’ translational potential for treatment approaches in ASD.
Link to the study : https://shorturl.at/Xbu31