Alzheimer’s disease (AD) is a prominent neurological disorder that predominantly impacts older people. It is also the primary cause of dementia. Given that aging is a major risk factor for AD, it is imperative that the disease be identified early in order to prevent irreversible cognitive impairment. Although there are currently no approved techniques for diagnosing AD in its early stages, recent studies suggest that electroencephalography (EEG) and the microbiota may play a role in early identification.
EEG is a non-invasive technique that measures brain activity and has the potential to distinguish between patterns in people with AD and mild cognitive impairment (MCI). This paper summarizes what is currently known about the microbiota and EEG as potential biomarkers for early-stage AD.
Key Findings
Alzheimer’s Disease and the Microbiome
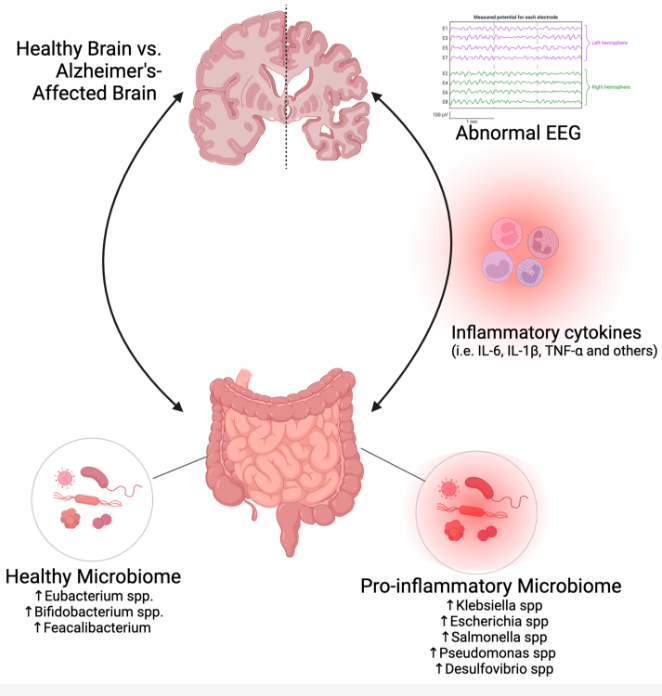
- Gut-Brain Axis: This is a bidirectional communication connection between the gut microbiota and the brain, with systemic inflammation being identified as a major link that contributes to AD. An imbalance in microbial communities, or gut dysbiosis, is more common in AD patients and causes increased gut permeability, systemic inflammation, and neuroinflammation.
- Oral Microbiome: AD risk is associated with chronic dental inflammation, such as periodontitis. The composition of the oral microbiome is altered in a distinctive way in AD patients, with higher concentrations of pathogenic bacteria including Aggregatibacter actinomyctemcomitans and Porphyromonas gingivalis as well as an increased abundance of Firmicutes and Fusobacteria.
- Gut Microbiome Composition: Individuals with AD have a lower diversity of microbes and unique microbiome signatures, such as a lower quantity of pro-inflammatory and amyloid-producing bacteria (like Klebsiella and Escherichia) and a higher quantity of pro-inflammatory and beneficial anti-inflammatory bacteria (like Bifidobacterium and Eubacterium).
- Microbial Metabolites: Trimethylamine N-oxide (TMAO), aromatic amino acids (AAAs), and short-chain fatty acids (SCFAs) are among the metabolites that the gut microbiota produces that influence brain function. For example, SCFAs reduce neuroinflammation and enhance brain function, whereas high levels of TMAO are linked to cognitive decline and a rise in the aggregation of tau and amyloid beta proteins in the brain.
Electroencephalography (EEG) and Alzheimer’s Disease
- EEG studies shows unique patterns in AD patients, such as a general slowing of brain activity marked by higher power in high-frequency bands (alpha and beta) and lower power in low-frequency bands (delta and theta).
- EEG measures such as spectral power ratio (SPR), complexity, and coherence can differentiate between AD, MCI, and cognitively healthy individuals. A lower SPR, for example, helps differentiate MCI from AD and denotes diminished cognitive performance.
- Patients with AD have gamma wave frequency alterations. It has been demonstrated that gamma stimulation can lessen AD symptoms and delay cognitive deterioration.
- Based on specific EEG slowing patterns and power distribution in distinct frequency bands, EEG can differentiate between different types of dementia, such as frontotemporal dementia (FTD) and dementia with Lewy bodies (DLB).
The microbiome and EEG show potential as non-invasive biomarkers for early detection of AD. Early diagnostic methods can be developed based on the unique microbiome signatures of AD patients and the particular EEG patterns seen in people with MCI. By combining microbiota and EEG data, early AD diagnosis could be more accurate and reliable, which could improve patient outcomes by allowing for immediate intervention.
Link to the study : https://tinyurl.com/2bavhdza