The escalation of antimicrobial resistance (AMR) due to the excessive and inappropriate use of antimicrobials has prompted the urgent need for more rapid and effective antimicrobial susceptibility testing (AST) methods. Conventional AST techniques often take 16–24 hours, leading to empirical prescription practices and the potential emergence of AMR.
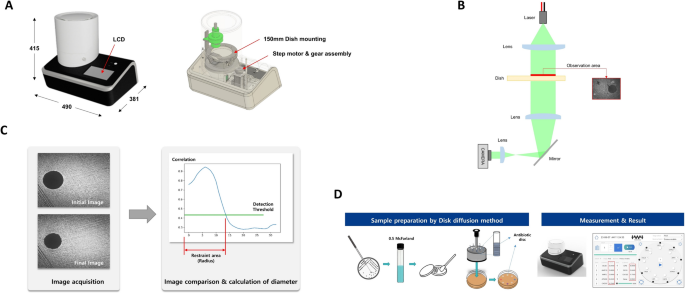
This study aimed to develop a rapid disk diffusion (RDD) method utilizing laser speckle formation (LSF) technology to expedite AST results. The performance of LSF technology was evaluated in determining antimicrobial susceptibility, comparing it with conventional disk diffusion (DD) methods in both preclinical and clinical settings.
Methods
- Study Design: The study involved preclinical and clinical experiments to evaluate the performance of LSF technology.
- Technology Utilized: LSF technology was applied to develop a rapid disk diffusion (RDD) method. This method uses laser speckle formation to measure inhibition zones quickly.
- Comparison: The LSF-based RDD method was compared with conventional DD methods to measure the inhibition zones of various antimicrobials.
- Bacterial Strains: Preclinical experiments involved different bacterial strains, while clinical experiments included multiple strains and antibiotics.
- Data Collection: Inhibition zones were measured, and categorical agreement (CA) between the LSF and DD methods was assessed. Major discrepancies (MD) and minor discrepancies (mD) were also recorded.
Key Findings
Preclinical Experiments:
- Categorical Agreement (CA): Demonstrated more than 70% CA against most antimicrobials.
- Specific Antimicrobials: Ampicillin, ampicillin-sulbactam, and aztreonam showed 100%, 81%, and 80% CAs, respectively, against E. coli. Cephalosporin and cefazolin had a high CA rate of 100%, while ceftazidime and cefepime showed 80% CAs.
- Concordance: High concordance between RDD and DD methods for multiple antimicrobials in multiple species.
Clinical Experiments:
- Categorical Agreement (CA): CA ranged from 40% to 79%.
- Discrepancies: Major discrepancies (MD) were observed around 30%, and minor discrepancies (mD) were around 11%.
- Specific Antimicrobials: Majority of antimicrobials in clinical studies demonstrated CAs as high as 78%.
Efficiency:
- The LS-AST device determined antimicrobial susceptibility in the shortest possible time of 4 hours, one of the quickest AST methods.
- The equipment setup in transmission mode prevented the laser from penetrating beneath the antibiotic disk, allowing accurate quantification of the inhibitory zone.
Potential Sources of Error:
- Response to Antimicrobials: Unstable responses (colony death after measurement) or initial susceptibility followed by growth over time.
- Culture Medium: Unpredictable changes, such as drying, could influence the diffraction pattern, leading to errors in measurement.
- Bacterial Colonies: Uneven distribution and slow growth rates might affect inhibition zone measurement.
The LS-AST method displayed significant accuracy across diverse bacterial strains and antimicrobial drugs. This technology has a higher application potential than previously developed methods, contributing to the ongoing effort to develop faster AST approaches essential for addressing AMR in clinical settings. Further study is required to address identified challenges and enhance findings, including evaluating the Minimum Inhibitory Concentration (MIC) to validate LS-AST observations.
Link to the article : https://tinyurl.com/n5vyb4wa