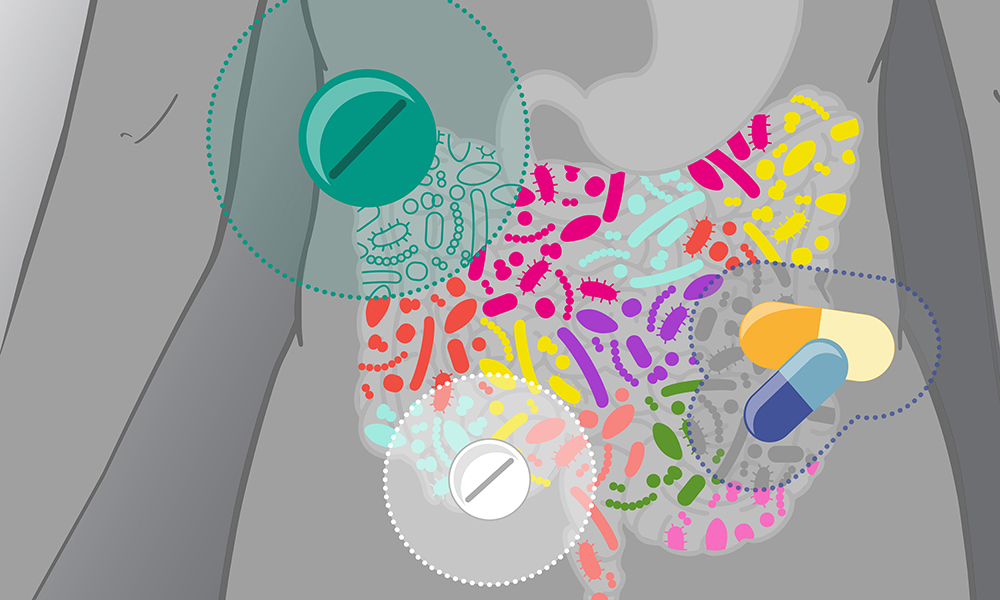
Antibiotic resistance (AR) poses a severe threat to global public health, claiming an estimated millions of lives globally. Resistance is acquired by bacteria either by horizontal gene transfer (HGT), in which genetic elements containing resistance genes are transferred between bacteria, or through mutations. The dynamics of AR are significantly influenced by the human gut microbiota, a varied ecology found in the gastrointestinal tract.
The gut microbiota, primarily composed of symbiotic bacteria, can harbor opportunistic pathogens. Importantly, the human gut microbiota serves as a reservoir for AR determinants, collectively known as the ‘gut resistome.’ Tetracycline, beta-lactam, and macrolide resistance genes are among the many types of AR genes found in the gut microbiota, as shown by high-throughput DNA sequencing. Interestingly, the gut microbiota can be disproportionately affected by antibiotics such as tetracyclines and macrolides, potentially impacting the resistome during therapy.
Among the prominent gut commensals, Bacteroides strains exhibit high resistance rates, particularly to beta-lactams and tetracyclines. The spread of AR within the gut microbiota is dynamic, as evidenced by the transmission of resistance genes like tetQ via conjugative transposons like CTnDOT. It is imperative to take actions to slow down the growth of the gut resistome.
Antimicrobial resistance (AMR) dynamics in the human body are largely influenced by the gut microbiome resistome, which is made up of intrinsic and mobile resistance genes. Through integration into mobile genetic elements, intrinsic resistance genes can become mobile-resistant even in the absence of prior exposure. Particular genomic regions known as Resistance Islands serve as an example of the intricacy of mobile resistomes. For instance, the 𝘈𝘤𝘪𝘯𝘦𝘵𝘰𝘣𝘢𝘤𝘵𝘦𝘳 𝘣𝘢𝘶𝘮𝘢𝘯𝘯𝘪 Resistance Island, an 86-kb genomic island, hosts 45 antimicrobial resistance genes, enabling microbes to resist antibiotics through various mechanisms such as disabling antibiotic influx, active efflux pump-driven antibiotic expulsion, modification of antibiotic target sites, and degradation of intracellular antibiotics. This highlights the intricate interplay between intrinsic and mobile resistance in the gut microbiome.
Understanding the factors that shape and spread ARGs in the gut microbiome is crucial due to its diverse regulatory role in the human body. The gut microbiota exhibits a dynamic nature due to its exposure to all foods and drugs taken, underscoring the necessity of cataloging ARGs for thorough investigation and problem-solving. One of the most important ways that ARGs spread across the gut microbiome is by conjugation, transduction, and transformation, or horizontal gene transfer (HGT) via MGEs.
In the mammalian gut, transformation—the reception of naked DNA from the surrounding environment—occurs infrequently, but if the acquired DNA contains ARGs, the bacterium becomes resistant. Within the same phylogenetic taxa, conjugation—which entails the creation of a mating bridge for ARG transfer—occurs more frequently. Notably, increased inflammation of the gut boosts ARG transfer between commensals and other pathogens. Conversely, in the healthy gut, intestinal epithelial cells produce compounds that hinder conjugation, reducing ARG transfer.
Transduction, where ARGs are encoded in bacteriophages incorporated into the host, emerges as a significant player in the gut resistome. This is corroborated by the quantity of bacteria and phages in the digestive system; research indicates that the phages of mice treated with antibiotics have higher ARG isolates. The complex relationship that exists between AMR and the gut microbiota highlights how crucial it is to comprehend these mechanisms in order to create focused plans of action for reducing the widespread problem of antibiotic resistance.
The misuse of antimicrobial drugs in medical, environmental, and animal settings has severely disrupted the gut microbiota’s natural community. This disruption shows up as increased bacterial translocation and mucus layer malfunction. As a result, these changed circumstances set off a series of immunological reactions that begin with dendritic cell activation. and macrophages through microorganism-associated molecular patterns (MAMPs) recognized by Toll-like receptors (TLRs). This recognition induces neutrophil chemotaxis and the production of interleukin (IL), leading to local inflammation and eventual damage to epithelial cells.
As a consequence of this immune activation, antigen-presenting cells (APC) present antigens to prime and sustain T-cell responses, while B cells inhibit the production of Ig A by plasma cells. Overall in all, the outcome is an inflammatory condition that eventually plays a role in the emergence of chronic illnesses. A number of treatment strategies have been investigated to mitigate these negative consequences. One possible treatment option for bacterial strain disruptions in the gut microbiota is phage therapy, which uses bacteriophages to target particular strains of the bacteria. Furthermore, it appears that fecal microbiota transplantation and the ingestion of functional foods enhanced with probiotics and prebiotics are viable approaches to reestablish homeostasis and a balanced microbiome. These therapies have the capacity to target specific bacterial taxa, providing a holistic approach to counteract the consequences of antimicrobial abuse on the gut microbiota and prevent the associated complications of chronic inflammation.
Further Reading:
Human microbiomes and antibiotic resistance : https://tinyurl.com/38rr73c7
Antibiotic resistance in the commensal human gut microbiota : https://tinyurl.com/3c8zrc5t
Metagenomics of Antimicrobial Resistance in Gut Microbiome : https://tinyurl.com/5n89hwbz
Potential Elimination of Human Gut Resistome by Exploiting the Benefits of Functional Foods : https://tinyurl.com/mwy3hs26