Brain Awareness Week 2023
Series 5 of 7
Brain-Gut-Microbiota Axis In Early-Life Development, Preterm Infants And Perinatal Depression.
Microbial colonization, and enteric nervous system maturation, coincide with the remodeling of brain neural circuits and cognitive development in the first years of life. The establishment of microbes in the Gastrointestinal tract can influence immune and metabolic mediators that ultimately may have an impact on the brain development and behavioral outcomes. Brain-Gut Axis has a major impact In early-life development, preterm infants and perinatal depression. Microbiome−based adjuvant therapies, administration of prebiotics, probiotics, and postbiotics supplements with nutritional and dietary interventions can alter the microbiota profile help maintain healthy gut microbiome and brain development.
- The development phases of the gastrointestinal (GI) tract and the brain are interdependent and occur in a parallel timeline in early-life.
- Microbial colonization, and enteric nervous system (ENS) maturation coincide with the remodeling of brain neural circuits and cognitive development in the first years of life
- The establishment of microbes in the GI tract can influence immune (e.g., microglia) and metabolic (e.g., neurotransmitters) mediators that ultimately may have an impact on the brain development and behavioral outcomes.
- The newborn gut microbiome is less diverse than that of the adult, the development of the gut microbiome is influenced by the gut-brain axis, and by maternal and neonatal exposures, including mode of delivery, antibiotic exposure, and feeding patterns.
- Preterm babies are exposed to increased stress levels that, in addition to an immature immune system, which may contribute to a higher susceptibility to infections, leading to therapeutic antibiotic treatments. These factors influence neurodevelopment either directly, by favoring inflammatory processes, or indirectly, by changing the composition of the gut microbiome.
- Perinatal depression is a mood disorder that is reported in women during pregnancy (prenatal) and after childbirth (postnatal). The onset of perinatal depression is associated with changes in reproductive hormones, stress hormones and neurosteroids.
- These chemical compounds can be modulated by the gut microbiota, which may affect maternal mental health during the perinatal period via the gut-brain-axis.
- Stress is known to activate the gut-brain, hypothalamic-pituitary-adrenal (HPA) axis, during and after pregnancy such activation is normally blunted, helping to insulate developing offspring from stress and dysregulation of the HPA axis has been suggested as playing a role in the physiology of perinatal depression.
- Microbiome−based adjuvant therapies, administration of prebiotics, probiotics, and postbiotics with nutritional and dietary interventions help alter microbiota profile, and help maintain healthy gut microbiome and brain development in infants, preterm-infants and in individuals with perinatal depression.
Further reading:
- The Infant Microbiome: Implications for Infant Health and Neurocognitive Development : bit.ly/3YRBTF7
- Priming for Life: Early Life Nutrition and the Microbiota-Gut-Brain Axis : bit.ly/3TmrFeI
- The Microbiota-Gut Axis in Premature Infants: Physio-Pathological Implications : bit.ly/3TDlnYB
- The microbiota-gut-brain axis and perceived stress in the perinatal period : http://bit.ly/3FxMIFs
- Gut microbiota: Linking nutrition and perinatal depression : bit.ly/3Fvu8hw
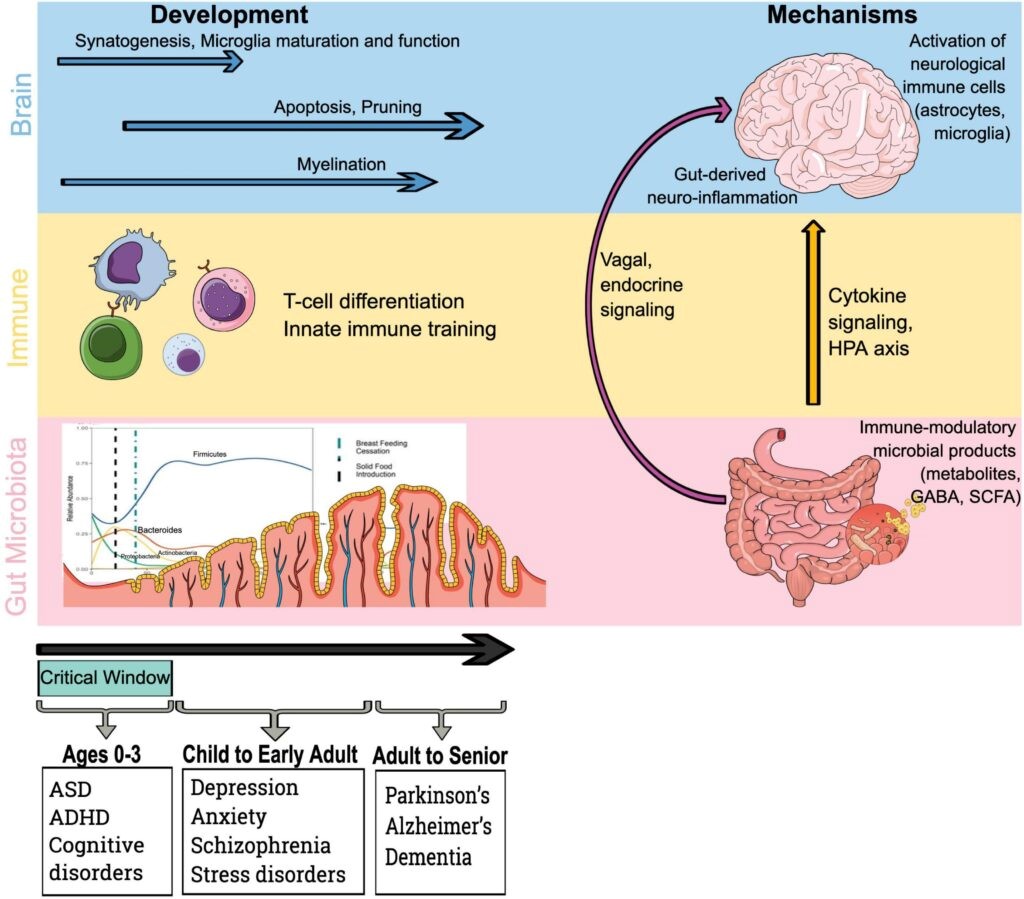
Microbiota, immune and brain development drive mechanistic pathways by which the gut microbiota influences the brain, Source: bit.ly/3FviIu7
Published On: 17/03/2023