Brain Awareness Week 2023
Series 3 of 7
Brain-Gut-Microbiota Axis In Alzheimer’s Disease.
Alzheimer’s disease (AD) is a neurodegenerative disease, that further leads to dementia.
Pathological hallmarks of AD include accumulation due to overproduction
and failure of clearance of amyloid-beta (Aβ) plaque, neuroinflammation, and neurofibrillary tangle formation. The Gut is a significant source of Aβ peptides, both the blood route and vagal nerve contribute to the transmission of intestinal Aβ and other substances into the brain, leading to neuroinflammation and neurodegeneration. This is aggravated in the case of the dysbiotic state of the gut. Microbiota-directed treatments (like diet, prebiotics, probiotics, and postbiotics) help maintain a healthy gut and may be a promising therapeutic approach to influence the development and progression of AD.
- Alzheimer’s disease (AD) is a neurodegenerative disease clinically defined by visual-spatial deterioration, extreme motor dysfunction , multi-domain cognitive impairment, further causing dementia.
- Pathological hallmarks of AD including accumulation due to overproduction and/or failure of clearance of amyloid-beta (Aβ) plaque, neuroinflammation and neurofibrillary tangle formation.
- Microglia induce phagocytosis in the Cental Nervous System(CNS), and results in the clearance of Aβ from the brain. Impairment of microglia function, facilitates the progression of AD and results in increased Aβ accumulation in the brain.
- Astrocytes are the most abundant glial subtype in the CNS, in their activated form (A1 astrocytes), express and release cytokines that modify the permeability of the Blood Brain Barrier, this is considered among the first steps in AD pathogenesis.
- Gut is a major source of Aβ peptides, bacterial amyloid can trigger misfolding and can enhance native amyloid aggregation. The gut microbiota products can activate microglia, which start neuroinflammation in the brain, causing loss of neurons, a major factor in AD.
- Patients with AD exhibit intestinal microbiota dysbiosis including decreased microbial richness and diversity, a low relative abundance of beneficial bacteria with the potential to synthesize short chain fatty acids, leading to neuroinflammation and neurodegeneration.
- Critical mechanisms of communication of the microbiota-gut-brain axis include: (1) the exposure of the brain to microbiota components (e.g., LPS, LTA), metabolites (e.g., SCFA, TMAO, neurotransmitters), and other products (e.g., EV) that can elicit an immune response and/or cross the BBB; (2) Microbiota-modification and metabolism of host products (e.g., bile acids); (3) secondary pathways affected by microbiota metabolism and byproducts (e.g., neuroendocrine signaling, vagus nerve)
- Microbiota-directed treatments (like diet, prebiotics, probiotics and postbiotics)help maintain healthy gut and may be a promising therapeutic approach to influence development and progression of AD.
Further Reading:
- Gut-derived β-amyloid: Likely a centerpiece of the gut–brain axis contributing to Alzheimer’s pathogenesis: bit.ly/40qH5RN
- Microglia and Astrocytes in Alzheimer’s Disease: Implications for Therapy: bit.ly/3Fp0GJK
- The Influence of the Gut Microbiota on Alzheimer’s Disease: bit.ly/3LjZzyW
- The Role of the Microbiota-Gut-Brain Axis in the Development of Alzheimer’s Disease: bit.ly/42h09nd
- The Microbiota–Gut–Brain Axis and Alzheimer Disease. From Dysbiosis to Neurodegeneration: bit.ly/3JjOJGl
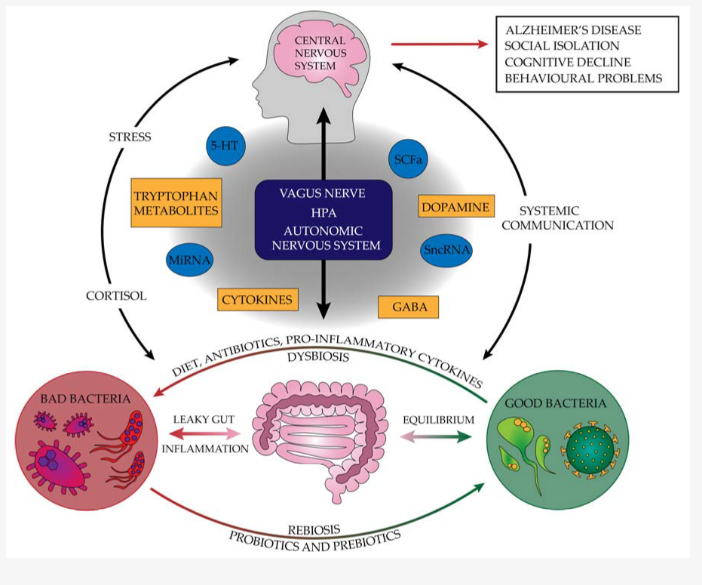
The pathogenesis of neurodegenerative diseases and factors protecting against their incidence that inhibit their progression (5-HT—serotonin, GABA—gamma-aminobutyric acid, HPA—hypothalamus–pituitary–adrenal, miRNA—microRNA, SCFAs—short-chain fatty acids, sncRNA—small non-coding RNA). Source: bit.ly/42h09nd
Published On: 15/03/2023