Acute Coronary Syndrome (ACS) is a critical subset of coronary artery disease characterized by episodes of angina, myocardial infarction, and sudden cardiac death. The prevalence of ACS has reached pandemic levels globally, posing a significant public health burden. Recent studies have suggested that the gut microbiome plays a role in the onset, progression, and treatment of ACS, influencing various cardiovascular risk factors. This study aims to investigate the changes in gut microbiota composition and metabolic pathways in ACS patients before and after treatment.
Methods
- Participants: 38 ACS patients undergoing percutaneous coronary intervention and statin therapy, along with 38 healthy controls who were family members.
- Sample Collection: Gut microbiota samples were collected from ACS patients at three time points: before treatment, one month after treatment, and two months after treatment.
- Sequencing: Shotgun metagenomic sequencing was used to analyze the gut microbiota, allowing for detailed identification of microbial species and metabolic pathways.
- Analysis: Differential species and metabolic pathways were examined to understand the impact of treatment on gut microbiota composition.
Key Findings
Microbial Composition Changes:
- Parabacteroides, Escherichia, and Blautia decreased after treatment.
- Gemalla, Klebsiella variicola, Klebsiella pneumoniae, and other species increased after treatment.
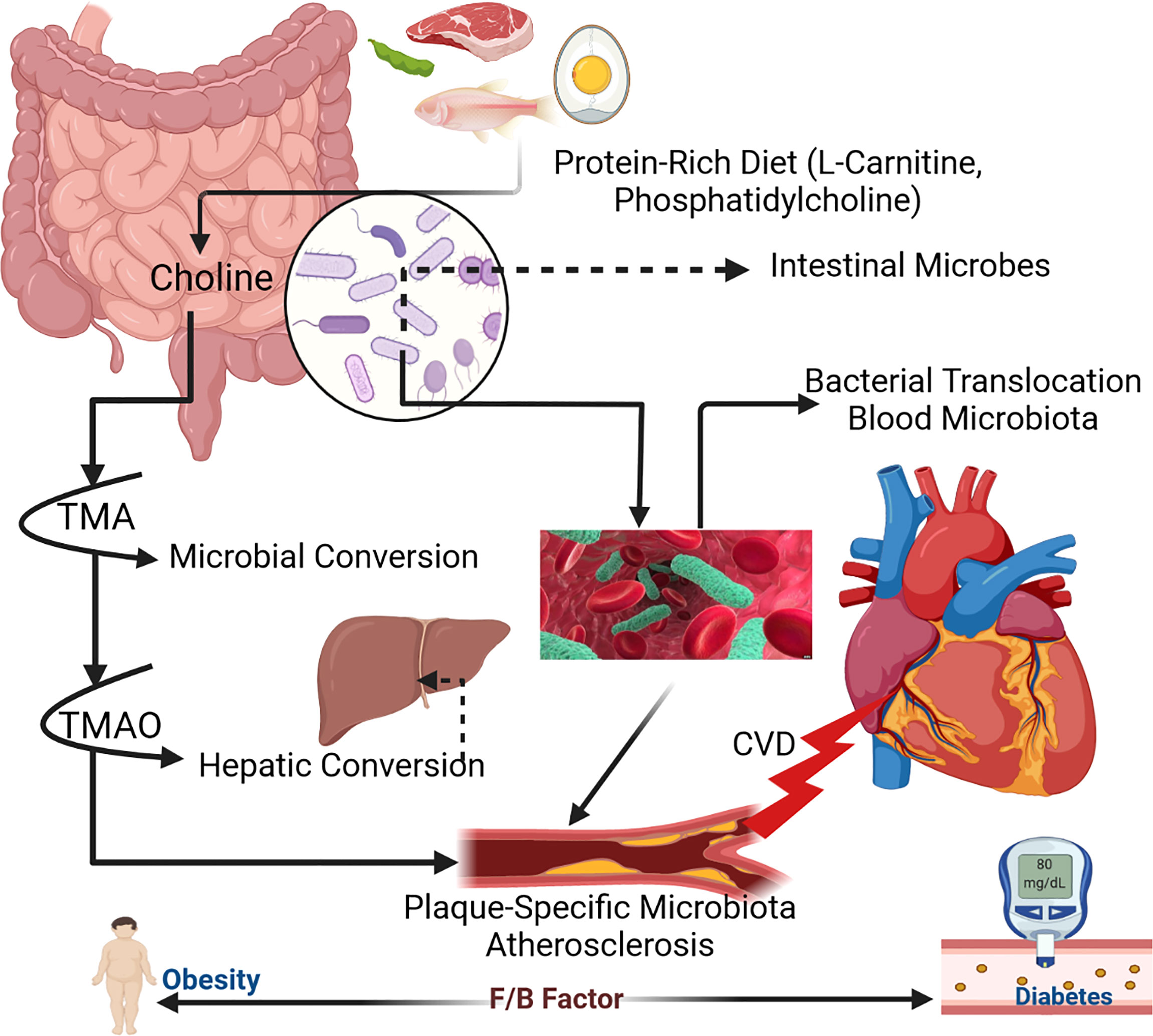
- Firmicutes/Bacteroidetes Ratio was lower in ACS patients compared to healthy controls but increased after therapy, indicating a potential restoration of gut microbiota balance.
Metabolic Pathways:
- Sugar Degradation Pathways: More abundant in patients before treatment, linked to disorders of sugar metabolism such as hyperglycemia, insulin resistance, and insufficient insulin secretion.
- Vitamin K2 Biosynthesis Pathways: Reduced after treatment, suggesting recovery from symptoms related to atherosclerosis and reduced need for vitamin K2 production.
Statin-Specific Effects:
- Rosuvastatin:
- Promoted the growth of anti-inflammatory bacteria such as Faecalibacterium prausnitzii.
- Reduced pro-inflammatory bacteria including Escherichia, Ruminococcus gnavus, and Veillonella parvula.
- Atorvastatin:
- Mixed effects on pro-inflammatory and anti-inflammatory bacteria.
- Increased abundance of Bacteroides genus.
- Decreased levels of both pro-inflammatory bacteria (e.g., Enterobacteriaceae) and anti-inflammatory bacteria (e.g., Blautia, Lactococcus).
- Other Significant Species:
- Increased in ACS Patients: Anaerotruncus colihominis, Clostridium evryensis, and Fusobacterium fastidiosum.
- Decreased in ACS Patients: Gemmiger formicilis, Eubacterium eligens, Bifidobacterium adolescentis, and Roseburia hominis.
Inflammatory and Anti-Inflammatory Balance:
- Firmicutes: Mainly produce butyrate, which has anti-inflammatory properties.
- Bacteroidetes: Produce acetate and propionate, with acetate potentially contributing to obesity and cardiovascular risk.
Metabolites Influencing Heart Health:
- Urolithin Production Decreased abundance of G. pamelaeae, which produces urolithin, an anti-atherosclerotic compound.
- Butyrate Production Reduced E. eligens, which inhibits obesity and prevents coronary heart disease.
This study provides insights into the changes in gut microbiota and metabolic pathways in ACS patients before and after treatment. The findings highlight specific bacterial species and pathways that may be associated with cardiovascular disease risk and offer potential therapeutic targets. Further research with larger sample sizes and animal experiments is necessary to validate these findings and understand the underlying mechanisms.
Link to the study : https://tinyurl.com/2d9ha8z7