The human gut microbiome plays a critical role in maintaining health by participating in various physiological processes. It is constantly exposed to external stimuli, including dietary compounds, pharmaceuticals, and xenobiotics, which can significantly affect its composition and function.
Historically, research has focused on the interaction between antibiotics and pathogenic microbes, but recent studies have highlighted that non-antibiotic drugs also affect the gut microbiome. This review explores how gut commensals respond to, resist, and recover from drug exposure, emphasizing the impact of both antibiotics and human-targeted drugs on the microbiome’s stability and resilience.
Methods
To review the survival strategies of gut commensals under drug exposure, the authors analyzed existing literature and experimental studies. The methodologies included:
- Systematic probing of the direct fitness effects of FDA-approved drugs on representative gut microbiome species.
- Ex vivo screening methods to assess changes in proteome and microbial community structures in response to human-targeted drugs.
- In vitro exposure of microbial species to various drugs to observe physiological changes and metabolic impacts.
- Use of synthetic communities and donor-derived microbial communities to study drug-microbiome interactions and community-level responses.
- Meta-analysis of cohort studies to examine the recovery of the microbiome after drug-induced perturbation.
Key Findings
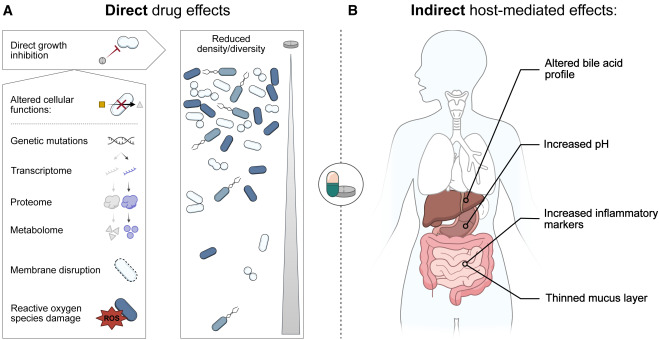
- Direct and Indirect Effects of Drugs: Both antibiotics and human-targeted drugs can directly inhibit microbial growth by disrupting metabolic processes, molecular machinery, or cellular structures. Indirect effects include changes in host physiology, such as altered bile acid metabolism or increased gastrointestinal pH, which in turn affect the microbiome.
- Microbial Resistance Mechanisms: Gut microbes employ various strategies to resist drugs, including decreased uptake, increased efflux, degradation of compounds, and modification of drug targets. Efflux pumps and enzymatic degradation play significant roles in microbial resistance.
- Community-Level Responses: In complex microbial communities, the response to drugs can lead to cross-sensitization or cross-protection. Cross-protection involves collective defense mechanisms, such as drug detoxification or bioaccumulation by specific community members, which protect sensitive species.
- Recovery and Resilience: Recovery of the gut microbiome post-drug exposure is influenced by the baseline composition of the community and the extent of perturbation. Factors such as functional and taxonomic diversity, presence of specific recovery-associated taxa, and external influences like social interactions play crucial roles in the restoration process.
- Therapeutic Interventions: Prebiotics, probiotics, and fecal transplants show promise in restoring microbial balance after drug-induced disruptions. However, their efficacy in the context of non-antibiotic drugs needs further investigation.
Understanding the interactions between drugs and the gut microbiome is vital for developing therapeutic strategies that consider the broader ecological context of the human microbiome. Future research should focus on elucidating the mechanistic basis of these interactions, exploring innovative interventions, and translating findings into clinical applications to enhance therapeutic efficacy and minimize adverse effects.
Link to the study : https://tinyurl.com/2p922jy9