Understanding the effects of medical interventions on the gut microbiome, resistome, and mycobiome of preterm infants is crucial for advancing infection prevention and treatment strategies. Researchers in this study conducted a prospective quasi-intervention study to investigate how antibiotics, probiotics, and other medical factors influence the gut development of preterm infants. Additionally, they employed a controlled neonatal mice model to predict and reflect exposures closely. This study aims to enhance our understanding of the impact of these interventions on the microbial communities of preterm infants.
Methods:
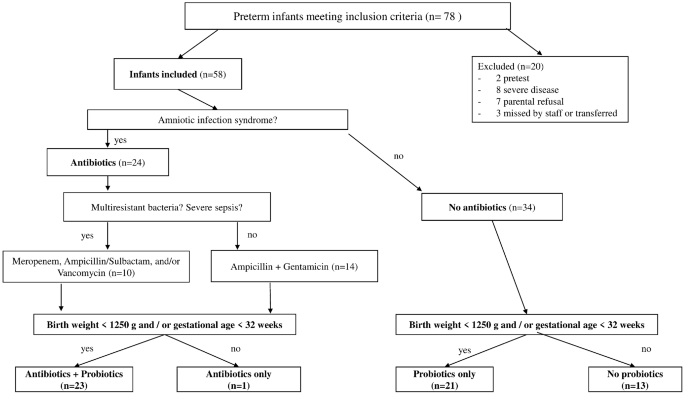
Preterm infants and neonatal mice were stratified into four groups: antibiotics only, probiotics only, antibiotics followed by probiotics, and no interventions. Stool samples were collected at various time points and analyzed using 16S rRNA amplicon sequencing, ITS amplicon sequencing, and whole-genome shotgun sequencing to assess the microbiome, mycobiome, and resistome. Statistical analyses were performed to identify significant differences between treatment groups.
Key Findings:
Human Infant Microbiomes:
- High heterogeneity was observed in the microbiomes of preterm infants.
- Little impact from medical exposure (antibiotics/probiotics) was observed on strain patterns.
- 𝘉𝘪𝘧𝘪𝘥𝘰𝘣𝘢𝘤𝘵𝘦𝘳𝘪𝘶𝘮 𝘣𝘪𝘧𝘪𝘥𝘶𝘮 was more abundant after exposure to probiotics, regardless of prior antibiotic administration.
Effects of Probiotics and Environmental Factors:
- 𝘉𝘪𝘧𝘪𝘥𝘰𝘣𝘢𝘤𝘵𝘦𝘳𝘪𝘶𝘮 𝘣𝘪𝘧𝘪𝘥𝘶𝘮 was significantly more abundant in the probiotics only and antibiotics paired with probiotics groups.
- Administration of antibiotics in combination with probiotics may rebalance and enrich the gut microbiome compositions.
- Environmental and genetic factors strongly influence gut development, as observed in twins/triplets.
Resistome Analysis:
- Twenty-seven antibiotic-resistant genes were identified in the resistome.
- Antibiotics only or antibiotics with probiotics exposure led to an increase in antibiotic resistance genes.
- Probiotics only group showed genes conferring resistance to certain antibiotics, suggesting potential environmental or genetic influences.
Mycobiome Analysis:
- Birthplace and multiple births significantly influenced alpha and beta diversity of the mycobiome.
- 𝘊𝘢𝘯𝘥𝘪𝘥𝘢 was the dominant genus in all treatment groups, suggesting vertical transmission from mothers.
Probiotic Effects in the Mouse Model:
- Transient effects of medical interventions were observed in both preterm infants and neonatal mice.
- Antibiotic treatment influenced gut compositions, but no lasting effects were detected.
- Probiotic administration resulted in transient alterations in gut compositions, with some associations with non-beneficial taxa.
While the analyses revealed transient effects of medical interventions on the gut microbiome, resistome, and mycobiome of preterm infants, these results provide positive motivation to continue research in this area. Environmental and genetic factors play significant roles in gut development, highlighting the need for further investigation.
Link to the article : https://tinyurl.com/3werb65e