As we age, the risk of cognitive decline and depression increases, impacting our overall well-being. A fascinating area of research suggests that the gut microbiome, the community of microorganisms living in our intestines, may play a crucial role in these conditions. A recent study delved into this connection, aiming to uncover how the gut microbiome influences cognitive function and depressive symptoms in older adults.
Key Findings:
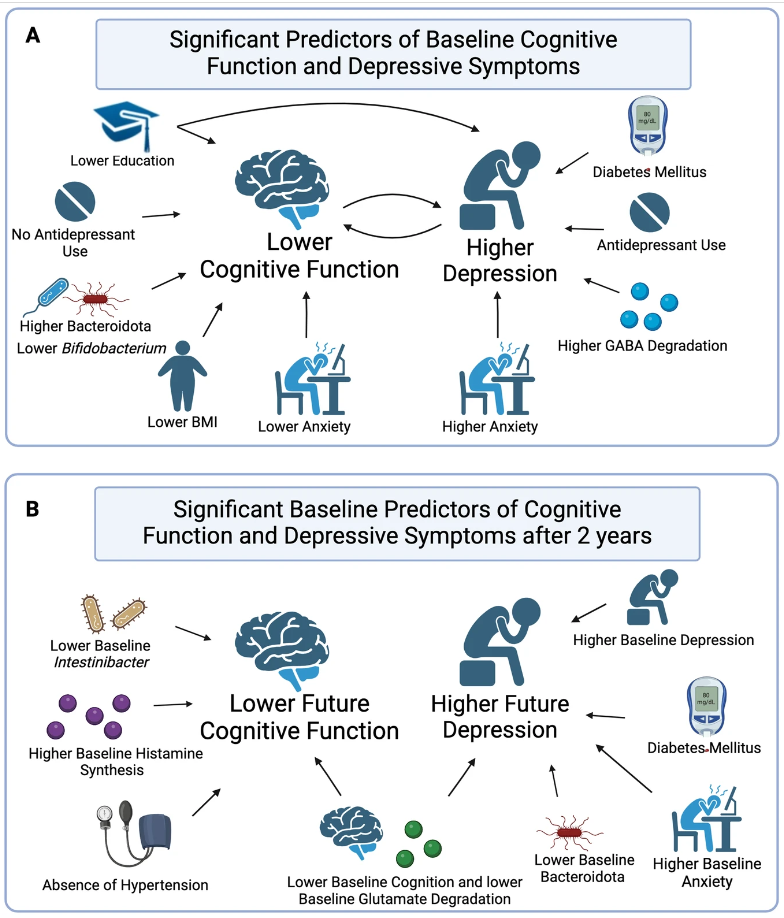
- Current Cognitive Function and Depression: The study found that greater diversity in the gut microbiome was associated with lower cognitive function and increased depression severity, particularly in individuals not taking antidepressants. This suggests that the composition of gut bacteria may influence our cognitive and emotional well-being.
- Microbial Composition and Cognitive Decline: Certain microbial features were linked to current cognitive function and predicted future cognitive decline. For example, lower levels of Bacteroidota and Bifidobacterium were associated with worse cognitive function. Interestingly, changes in microbial metabolism, such as glutamate degradation, were also linked to cognitive decline.
- Microbial Composition and Depressive Symptoms: Similarly, the study found associations between microbial composition and depressive symptoms. Higher depression severity was linked to specific microbial features, including increased GABA degradation. GABA is a neurotransmitter involved in mood regulation, suggesting a potential link between gut bacteria and depressive symptoms.
- Predictive Value of the Microbiome: Importantly, the study revealed that the gut microbiome could predict future cognitive decline and depressive symptoms. Changes in microbial composition observed at baseline were associated with changes in cognitive function and mood two years later, highlighting the potential of the microbiome as a biomarker for these conditions.
Implications and Future Directions:
This study sheds light on the intricate relationship between the gut microbiome, cognitive function, and depressive symptoms in older adults. Understanding these connections could lead to personalized treatment approaches aimed at altering disease progression and improving quality of life for older individuals.
However, the study also has limitations, including its non-probabilistic sampling method and predominantly female sample. Further research is needed to validate these findings in more diverse populations and to explore the underlying mechanisms driving the interactions between gut bacteria and brain health.
Link to the article : https://tinyurl.com/4dt9samd