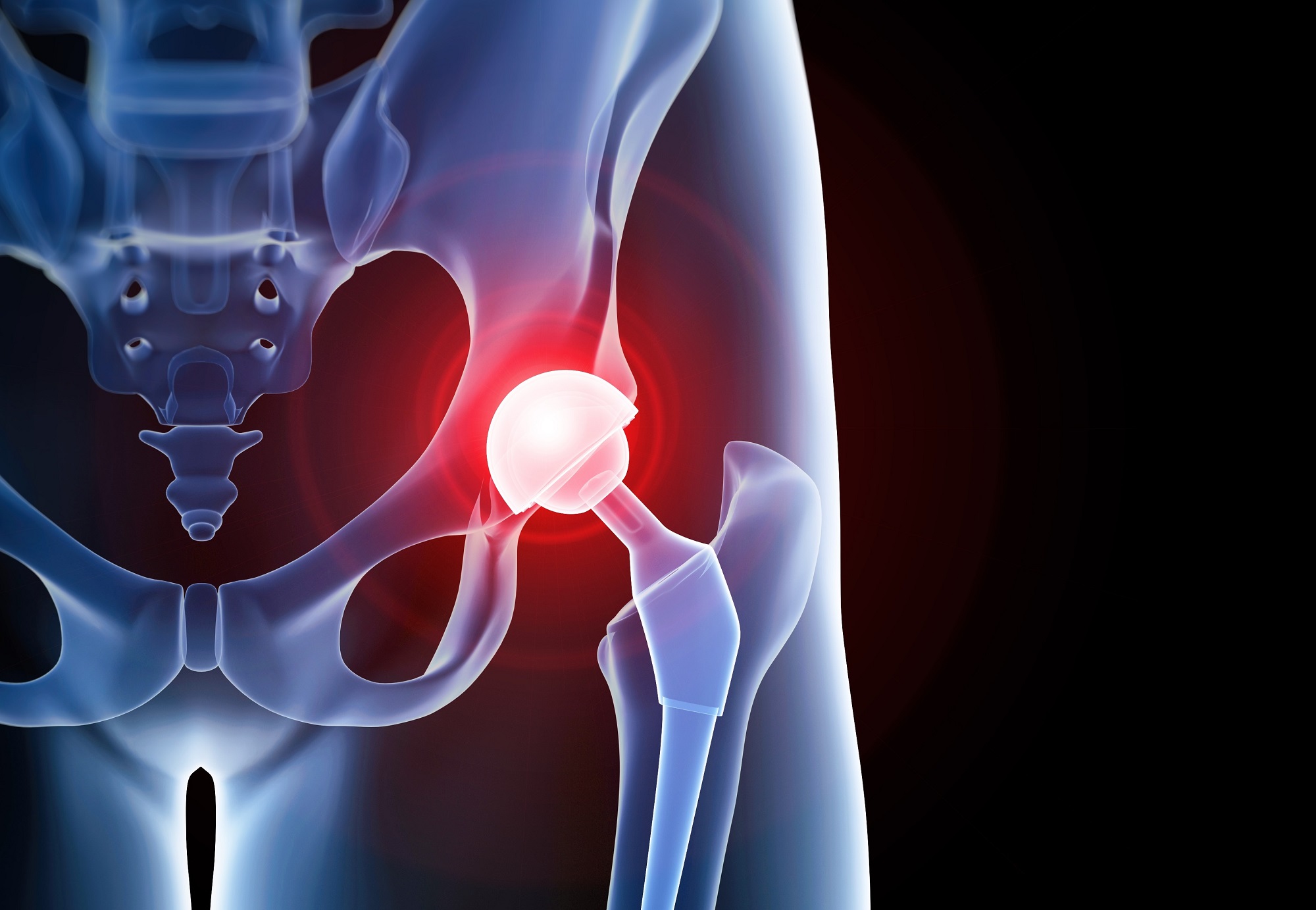
Periprosthetic joint infection (PJI) is a serious complication of joint replacement surgery, particularly total joint arthroplasty. Recent evidence suggests a potential link between dysregulation of the gut microbiota and joint degenerative diseases, prompting investigation into how the presurgical gut microbiota may influence susceptibility to PJI. This report delves into the scientific findings related to the microbiome’s role in PJI, associated treatment strategies, and emerging therapies targeting microbiome restoration
Microbiome Dysbiosis and PJI Risk:
- The gut microbiota’s dysregulation may elevate the risk of PJI, possibly by facilitating bacterial translocation or impairing immune responses.
- Presurgical gut microbiota influences infection resistance, highlighting a previously overlooked factor in PJI pathogenesis.
- Factors such as genetics, health status, lifestyle, diet, antibiotics, and sanitation practices contribute to microbiome dysbiosis.
Microbial Factors in PJI Pathogenesis:
- Common causative agents of PJI include coagulase-negative staphylococci, Staphylococcus aureus, streptococci, enterococci, Enterobacterales, and Propionibacteria.
- Polymicrobial infections, characterized by multiple simultaneous organisms infecting a single prosthesis, are associated with unfavorable outcomes.
- The timing and route of infection can classify PJIs into early, delayed, or late categories, each requiring specific diagnostic and treatment approaches.
Diagnostic Approaches:
- Tissue biopsy and invasive procedures for PJI diagnosis may be replaced by non-invasive indicators like gut microbiota species and metabolites.
- Fecal samples and microbiota species profiling can serve as non-invasive diagnostic tools for identifying dysbiosis.
- Standardizing PJI definitions and diagnostic algorithms is crucial for efficient and cost-effective patient assessment.
Treatment Strategies:
- Proper surgical procedures and antibacterial concepts are essential for successful PJI therapy.
- Surgical approaches include debridement, antibiotic therapy, and implant retention (DAIR), one-stage, two-stage, or three-stage revision surgeries.
- Challenges in revision surgeries underscore the importance of careful patient selection and a multidisciplinary, patient-centered approach.
Complications and Factors Influencing Treatment:
- Culture-negative PJI cases pose challenges, emphasizing the need for identifying the infecting organism.
- Duration of postoperative antibiotic regimens lacks uniformity; chronic antibiotics may impact the microbiome.
- The gut microbiome’s link to PJI suggests potential preventive therapies targeting microbiome restoration.
Emerging Therapies:
- Microbiome-based therapies, including probiotics, prebiotics, synbiotics, and fecal microbiota transplantation, offer innovative approaches to restore microbial balance.
- Exercise, dietary modifications, and emerging therapies like phage therapy and predatory bacteria show promise in microbiome modulation.
- Gut microbiome manipulation may become a routine postoperative care element to promote microbiome restoration after surgery.
The gut microbiome’s role in PJI is a promising area of research, with potential implications for preventive strategies. Modifying patients’ microbiomes preoperatively could reduce PJI risk, opening new avenues for personalized and targeted interventions. Further research is needed to explore microbiome-based therapies and optimize their application in joint replacement surgeries. The evolving understanding of microbiome dynamics creates opportunities for precision medicine in PJI prevention and treatment.
Link to the study : https://tinyurl.com/39n3hfbv