💡 This study delves into the complex interplay between gut microbiota, metabolites, and immune cell subsets in Unexplained Recurrent Spontaneous Abortion (URSA), a challenging clinical condition with elusive etiology. Through an integrative approach, the study establishes connections between alterations in gut microbiota diversity, specific metabolite levels, and immune cell subset frequencies in URSA patients.
📍 Key Scientific Findings:
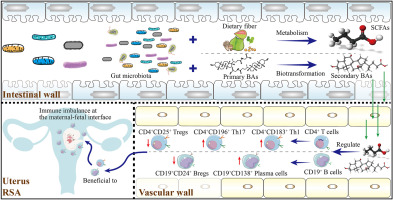
📌 Gut Microbiota Alterations in URSA: Reduced diversity and distinct bacterial genera observed in the gut microbiota of URSA patients. Potential dysbiosis identified, suggesting a link between altered microbiota composition and immune dysregulation in URSA.
📌 Metabolomic Profiling in URSA: Targeted metabolomic analysis reveals decreased levels of gut microbiota-derived metabolites, including deoxycholic acid (DCA), glycolithocholic acid (GLCA), acetate, propionate, and butyrate in URSA patients. Significance of these metabolites in physiological processes and their impact on the immune system highlight their potential role in URSA pathogenesis.
📍 Immune Dysregulation in URSA:
📌 Altered frequencies of immune cell subsets in peripheral blood of URSA patients: Increased Th1, Th17, and plasma B cells, Decreased Tregs and Bregs. Reflects an immune response imbalance associated with URSA.
📌 Correlation Between Metabolites and Immune Cell Subsets: Strong correlations established between gut microbiota-derived bile acids (BAs) and short-chain fatty acids (SCFAs) levels and immune cell subset frequencies in circulation. Implicates potential mechanistic links between altered metabolites and immune cell dysregulation in URSA.
📍 Mechanistic Insights into Metabolite-Immune Interactions:
📌 Preliminary insights into how SCFAs and BAs impact immune cell function: SCFAs influence immune tolerance, inflammatory responses, and T cell and B cell differentiation. BAs, by activating specific receptors, may suppress inflammatory Th1 and Th17 responses.
📍 Chicken or Egg Dilemma: Gut Dysbiosis and Immune Dysfunction: The study explores the bidirectional relationship between gut microbiota dysbiosis and immune dysfunction in URSA. The mutual reinforcement of gut microbiota alterations and immune dysregulation forms a complex interplay, contributing to URSA pathogenesis.
This comprehensive investigation unveils significant associations between gut microbiota alterations, metabolite levels, and immune dysregulation in URSA. The findings provide valuable insights into potential mechanisms contributing to URSA pathogenesis, paving the way for future therapeutic interventions and emphasizing the pivotal role of the gut-immune axis in reproductive health.
Link to the study : http://tinyurl.com/384vjc56