💡 Battles against microscopic pathogens and the scorching wrath of Mother Earth may seem worlds apart, but what if they share more in common than we thought?
The revolutionary discovery of penicillin birthed superbugs, resistant to our once powerful antibiotics, due to overuse. Today, these superbugs are a global health crisis, disrupting treatments and spreading rapidly among humans and animals. Concurrently, climate change alters habitats and disease ranges, heating our world and straining vulnerable species. The interplay between these two existential threats complicates their individual impacts.
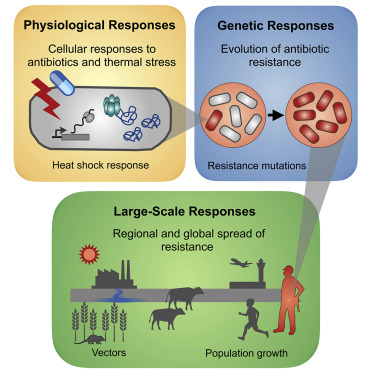
The researchers found that climate change and superbugs are not separate crises, but closely intertwined. As global temperatures rise, bacteria grow faster, facilitating the exchange of resistance genes. This creates an ideal environment for superbugs to evolve, survive, and expand, intensifying the threat we face. Adding another twist to this complex tangle are rising incidences of new and re-emerging pathogens. As global conditions morph, diseases once confined to textbooks could find a disturbing resurgence. As temperatures rise, scientists worry that waterborne diseases such as cholera and salmonella may become increasingly prevalent and antibiotic-resistant. Concurrently, vector-borne diseases, typically confined to tropical climates, could extend their grasp, reaching areas previously unthreatened.
📍 Examples of few infections due to climate change is mentioned below:
𝘊𝘢𝘮𝘱𝘺𝘭𝘰𝘣𝘢𝘤𝘵𝘦𝘳 𝘴𝘱𝘱. 𝘢𝘯𝘥 𝘚𝘢𝘭𝘮𝘰𝘯𝘦𝘭𝘭𝘢 𝘴𝘱𝘱 : Rising temperatures in water systems contribute to the better survival of these microorganisms, leading to waterborne and foodborne diseases.
𝘊𝘢𝘯𝘥𝘪𝘥𝘢 𝘢𝘶𝘳𝘪𝘴 : This fungus has shown increased thermo-tolerance and survival rates in warmer temperatures, leading to a rise in fungal infections.
𝘗𝘭𝘢𝘴𝘮𝘰𝘥𝘪𝘶𝘮 𝘧𝘢𝘭𝘤𝘪𝘱𝘢𝘳𝘶𝘮 : Rising temperatures and humidity contribute to increased transmissibility of the malaria parasite.
Zika, Chikungunya, and Dengue viruses, 𝘛𝘳𝘪𝘱𝘢𝘯𝘰𝘴𝘰𝘮𝘢 𝘤𝘳𝘶𝘻𝘪: Warmer temperatures have led to the increased spread of vectors (like mosquitos) carrying these pathogens, even in previously colder regions, leading to a rise in vector-borne diseases.
𝘗𝘴𝘦𝘶𝘥𝘰𝘮𝘰𝘯𝘢𝘴 𝘢𝘦𝘳𝘶𝘨𝘪𝘯𝘰𝘴𝘢, 𝘒𝘭𝘦𝘣𝘴𝘪𝘦𝘭𝘭𝘢 𝘱𝘯𝘦𝘶𝘮𝘰𝘯𝘪𝘢𝘦, 𝘌𝘴𝘤𝘩𝘦𝘳𝘪𝘤𝘩𝘪𝘢 𝘤𝘰𝘭𝘪, 𝘢𝘯𝘥 𝘚𝘵𝘢𝘱𝘩𝘺𝘭𝘰𝘤𝘰𝘤𝘤𝘶𝘴 𝘢𝘶𝘳𝘦𝘶𝘴 : The warm-season changes in temperature influence the optimal growth conditions of these Gram-negative bacteria, contributing to a rise in such infections, especially in healthcare settings.
SARS-CoV-2: Climate change-induced aridity and prolonged droughts contribute to bat migration, subsequently escalating the spread of SARS-CoV-2.
Addressing the intertwined challenge of AMR and climate change necessitates integrated strategies like the One Health approach, which acknowledges the interconnections between human, animal, and environmental health. The COVID-19 pandemic, emphasizing these links with its worldwide spread and consequent antibiotic surge, reinforces the need for this consolidated approach.
What can we do?
To address the interlinked challenges of antimicrobial resistance and climate change, a comprehensive, multi-pronged approach is necessary. It starts with robust policy and regulation where governments play a central role in controlling antibiotic misuse in both medical and agricultural sectors. Implementing antimicrobial stewardship in hospitals and other healthcare facilities can promote judicious use of antibiotics while minimizing unnecessary prescriptions. Public awareness campaigns are also key in educating the masses about the dangers of antibiotic misuse and the realities of climate change. Additionally, investing in research and development can pave the way for new antibiotics and renewable, sustainable energy sources to combat both crises. Tackling the environmental aspects involves concerted efforts to reduce greenhouse gas emissions, promote the use of cleaner energy sources, limit deforestation, and encourage sustainable practices. Emphasizing the One Health Approach, which acknowledges the interdependency of human, animal, and environmental health, can help guide holistic actions beneficial to all three sectors. It’s crucial to note that these diverse actions must be implemented together, as no single solution can effectively combat these complex, interconnected crises.
References:
- Gudipati, S.; Zervos, M.; Herc, E. Can the One Health Approach Save Us from the Emergence and Reemergence of Infectious Pathogens in the Era of Climate Change: Implications for Antimicrobial Resistance? Antibiotics 2020, 9, 599.
- Omazic, A.; Bylund, H.; Boqvist, S.; Högberg, A.; Björkman, C.; Tryland, M.; Evengård, B.; Koch, A.; Berggren, C.; Malogolovkin, A.; et al. Identifying climate-sensitive infectious diseases in animals and humans in Northern regions. Acta Vet. Scand. 2019, 61, 53.
- Semenza, J.C.; Menne, B. Climate change and infectious diseases in Europe. Lancet Infect. Dis. 2009, 9, 365–375.
- Casadevall, A.; Kontoyiannis, D.P.; Robert, V. On the Emergence of Candida auris: Climate Change, Azoles, Swamps, and Birds. mBio 2019, 10, e01397-19
- Jones, G.; Rebelo, H. Responses of bats to climate change: Learning from the past and predicting the future. In Bat Evolution,Ecology, and Conservation; Springer: New York, NY, USA, 201
- Chaves, L.F.; Koenraadt, C.J. Climate change and highland malaria: Fresh air for a hot debate. Q. Rev. Biol. 2010, 85, 27–55.
- Magnano San Lio R, Favara G, Maugeri A, Barchitta M, Agodi A. How antimicrobial resistance is linked to climate change: an overview of two intertwined global challenges. International journal of environmental research and public health. 2023 Jan 17;20(3):1681.
- Tariq KA. Antimicrobial Resistance, Climate Change, and Public Health. Climate Change and Microbial Diversity. 2022 Aug 18:109.