Myasthenia gravis (MG) is an autoimmune disorder characterized by muscle weakness and fatigability.
💡 This study aimed to investigate whether there is a bidirectional causal relationship between gut microbiota composition and MG and to explore the mechanisms underlying the gut microbiota’s role in MG risk reduction.
📍 Methods:
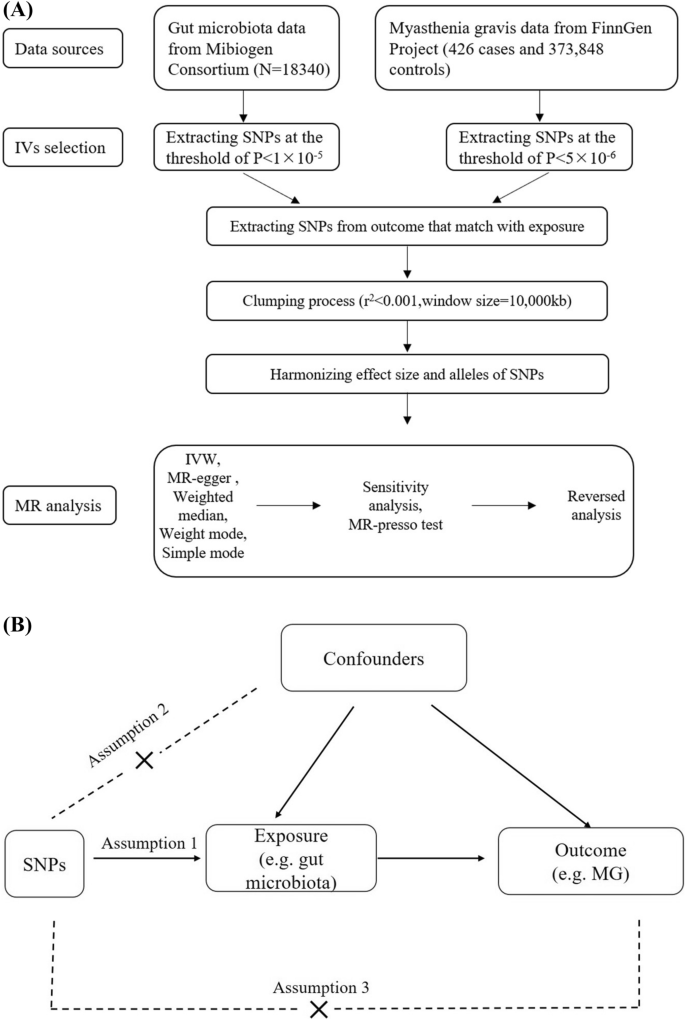
📌 Gut microbiota data was obtained at various taxonomic levels from a large cohort (N = 18,340) in the MiBioGen consortium and MG data from the FinnGen Research Project (426 MG cases and 373,848 controls).
📌 Two-sample Mendelian randomization (MR) analyses were performed to assess causal relationships between gut microbiota and MG. Bidirectional MR analyses were conducted to determine the direction of causality.
📌 Additionally, MR-Egger intercept and Cochran’s Q test were used to assess pleiotropy and heterogeneity, while MR-PRESSO was utilized to detect outliers.
📍 Key Findings:
📌 In the forward MR analysis, the genus Lachnoclostridium was positively correlated with an increased risk of MG (OR = 2.431, 95% CI 1.047–5.647, p = 0.039). In contrast, several microbial families and an unknown genus (Clostridiaceae1, Defluviitaleaceae, Enterobacteriaceae) exhibited negative correlations with MG risk, indicating a potential protective role.
📌 The reverse MR analysis revealed a negative association between MG risk and the presence of the genus Barnesiella (OR = 0.945, 95% CI 0.906–0.985, p = 0.008), suggesting that Barnesiella may play a protective role in MG development.
📌 Mechanistically, our findings indicate that specific gut microbiota components, such as Clostridium and Streptococcus, could promote the differentiation of naive CD4+ T cells into antigen-specific Foxp3+CD4+ Treg cells, thus increasing their numbers. This phenomenon may contribute to reducing MG risk.
📌 Short-chain fatty acids (SCFAs) produced by gut microbiota play a crucial role in regulating immune responses and maintaining immune homeostasis. SCFAs can directly influence the differentiation of T cells into Foxp3+CD4+ Treg cells, which could provide a protective effect against MG.
📍These findings suggest that targeting gut microbiota to increase the number of Foxp3+CD4+ Treg cells could be a novel approach for treating MG.
This study underscores the intricate interplay between gut microbiota and MG, offering new insights into the pathogenesis and treatment possibilities for this autoimmune disorder.
Link to the article : https://tinyurl.com/4dkknve5