💡 This prospective cohort study investigates the intricate relationship between psychosocial stress, depressive symptoms, and the dynamics of fecal and vaginal microbiota in pregnant individuals. Findings reveal unique shifts in microbial composition associated with stress and depression, suggesting distinct biological pathways. Notably, the study identifies specific microbial taxa, previously unlinked to pregnancy or stress, and explores potential mechanisms underlying the observed changes. The study also highlights the complex interplay between psychometric responses and microbial abundance across different stages of pregnancy and postpartum.
📍 Pregnancy is a period of heightened vulnerability to psychosocial stress and mood-related disorders. This study explores the impact of stress and depressive symptoms on the gut and vaginal microbiota, drawing on the gut microbiota-brain axis and associated signaling pathways. While prior research indicates alterations in maternal gut microbial composition due to prenatal stress, this study extends the understanding by employing a comprehensive cohort design, incorporating psychometric assessments and advanced sequencing techniques.
📍 Methods:
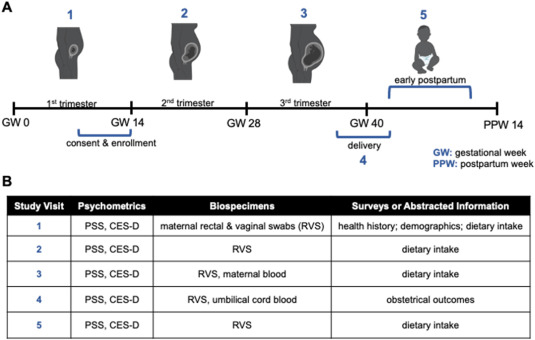
The study utilizes repeated psychometric assessments (Perceived Stress Scale and Center for Epidemiological Studies Depression Scale) and microbiome samples from fecal and vaginal sources throughout pregnancy. Full-length 16S rRNA sequencing, α and β-diversity metrics, and taxonomic abundance analyses are employed to characterize microbial community composition.
📍 Key Scientific Findings:
📌 Stress-Induced Fecal Taxa Shifts: Early pregnancy stress associates with increased abundance of fecal taxa, including 𝘍𝘢𝘦𝘤𝘢𝘭𝘪𝘵𝘢𝘭𝘦𝘢, 𝘊𝘢𝘵𝘦𝘯𝘪𝘣𝘢𝘤𝘵𝘦𝘳𝘪𝘶𝘮 𝘮𝘪𝘵𝘴𝘶𝘰𝘬𝘢𝘪, 𝘢𝘯𝘥 𝘚𝘵𝘳𝘦𝘱𝘵𝘰𝘤𝘰𝘤𝘤𝘶𝘴 𝘱𝘢𝘴𝘵𝘦𝘶𝘳𝘪𝘢𝘯𝘶𝘴, previously unlinked to pregnancy or stress.
2nd trimester stress is linked to elevated abundance of fecal 𝘗𝘳𝘦𝘷𝘰𝘵𝘦𝘭𝘭𝘢, contrasting with some non-pregnant studies, indicating the context-dependent role of 𝘗𝘳𝘦𝘷𝘰𝘵𝘦𝘭𝘭𝘢, in mental health.
📌 CCL2 and 𝘓𝘢𝘤𝘵𝘰𝘣𝘢𝘤𝘪𝘭𝘭𝘪 Dynamics: Maternal CCL2 concentrations during late pregnancy correlate with psychometric scores, while umbilical CCL2 inversely associates with fecal Lactobacilli at delivery.
Implications for the interplay between pro-inflammatory chemokines and beneficial Lactobacilli in stress and depression contexts are discussed.
📌 Vaginal Microbiota Responses to Stress: Stress during the 3rd trimester corresponds to increased abundance of fecal 𝘓𝘢𝘤𝘵𝘰𝘣𝘢𝘤𝘪𝘭𝘭𝘶𝘴, 𝘴𝘱𝘦𝘤𝘪𝘧𝘪𝘤𝘢𝘭𝘭𝘺 𝘓. 𝘪𝘯𝘦𝘳𝘴, suggesting stress-induced transmission of vaginal microbes to the gut.
Postpartum stress correlates with heightened abundance of fecal 𝘎𝘢𝘳𝘥𝘯𝘦𝘳𝘦𝘭𝘭𝘢, 𝘚𝘯𝘦𝘢𝘵𝘩𝘪𝘢 (𝘦𝘴𝘱𝘦𝘤𝘪𝘢𝘭𝘭𝘺 𝘚. 𝘢𝘮𝘯𝘪𝘪), 𝘈𝘤𝘵𝘪𝘯𝘰𝘮𝘺𝘤𝘦𝘴, 𝘚𝘤𝘩𝘢𝘢𝘭𝘪𝘢 (𝘚. 𝘵𝘶𝘳𝘪𝘤𝘦𝘯𝘴𝘪𝘴), 𝘢𝘯𝘥 𝘔𝘦𝘨𝘢𝘴𝘱𝘩𝘢𝘦𝘳𝘢 𝘦𝘭𝘴𝘥𝘦𝘯𝘪𝘪, previously associated with vaginal and gastrointestinal health.
📌 Depressive Symptoms and Dietary Microbiota Associations: Moderate depressive symptoms in mid-pregnancy correlate with decreased abundance of 𝘌𝘳𝘺𝘴𝘪𝘱𝘦𝘭𝘢𝘵𝘰𝘤𝘭𝘰𝘴𝘵𝘳𝘪𝘥𝘪𝘶𝘮, indicating potential links between diet, depressive symptoms, and microbial composition.
📌 Vaginal Diversity Dynamics: Participants with severe depressive symptoms experience a steeper decrease in vaginal α-diversity from early to late pregnancy, highlighting potential associations between mood disorders and vaginal microbial dynamics.
📍 This study provides a comprehensive exploration of the intricate relationships between psychosocial stress, depressive symptoms, and the dynamics of fecal and vaginal microbiota during pregnancy. The identified microbial taxa, associations, and potential mechanisms contribute valuable insights, paving the way for further mechanistic interrogations and targeted interventions to understand and address the complex interplay between mental health and microbial communities in pregnant individuals.
Link to the article : http://tinyurl.com/ys795mk7